WHAT'S NEW?
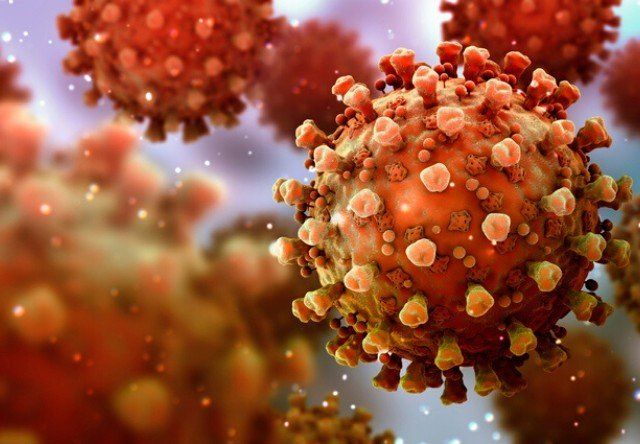
Coronavirus-induced disease-2019 (COVID-19) continues to cause significant morbidity and mortality worldwide. While studies on SARS-CoV-2 effects on immune cell function continue to progress, we know very little about the significance of depletion of key immune effectors by the virus in the mortality and morbidity of the disease. This commentary outlines what is the reported literature thus far on the effect of virus on NK cells known to kill virally infected cells. It also underscores the necessity for the future comprehensive studies of NK cells in SARS-CoV-2 infected individuals and animal models to better understand the role and significance of reported NK cell depletion and functional inactivation in disease morbidity and mortality, in hope to design effective therapeutic interventions for the disease. Coronavirus-induced disease-2019 (COVID-19) poses a great public health threat, and presents a complex challenge for epidemiologists and public health professionals around the planet, as the disease has shifted from a regional epidemic to a worldwide pandemic in a short period of time. The toll that the disease has had on the global level continues to increase as the virus reaches all continents, except Antarctica, afflicting more than 180 countries. Initial reports of COVID-19 disease came from Wuhan, China in late December 2019, as patients began complaining about unexplained respiratory infections, which later was coined as “pneumonia of unknown etiology” (1). Shortly after surfacing of the virus several independent laboratories identified the causative agent of COVID-19 disease, ultimately naming it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (2, 3). While the search is continuing to uncover the infectious path of SARS-CoV-2, several key findings have led the infectious disease experts to partly uncover the mechanisms of the original spread to humans. By phylogenetically comparing SARS-CoV-2 to other coronaviruses, it was noted that the new virus was highly identical to other coronaviruses that had originated from bats (3, 4). However, to date the complete transmission route remains elusive. Despite the novelty of this particular strain of coronavirus, the SARS-CoV-2 is not without precedent. Outbreaks in the past decades, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), identified viruses that fall into the same category of coronaviruses, which are single-stranded RNA viruses (+ssRNA) that morphologically have been determined to express crown-like spikes on their surfaces. However, the difference seen between prior species of coronaviruses and SARS-CoV-2 partly lies in their respective symptom presentations in patients. Compared to SARS and MERS, the symptoms of COVID-19 disease are not presented earlier in the infectious cycle, which may be a reason for the greater ability of viral transmission in patients (4). The incubation period of the SARS-CoV-2 is relatively longer than those of SARS and MERs (7–14 days vs. 5.0–6.9 and 4.4–6.9, respectively) (4). In addition to its longer incubation period, the mean reproductive number (R0) of SARS-CoV-2 has also been estimated to range from 2.20 to 3.58, indicating that each infected patient can on average transmit the disease to two to three other individuals (5, 6). Read the Full Publication Click Here, or Go To - https://www.frontiersin.org/articles/10.3389/fimmu.2020.01692/full
Division of Oral Biology and Medicine, The Jane and Jerry Weintraub Center for Reconstructive Biotechnology, UCLA, Los Angeles, CA; bThe Jonsson Comprehensive Cancer Center, UCLA School of Dentistry and Medicine, Los Angeles, CA; cDepartment of Biotechnology, Jožef Stefan Institute, Ljubljana, Slovenia; dFaculty of Pharmacy, University of Ljubljana, Ljubljana, Slovenia; eDepartment of Genetic Toxicology and Cancer Biology, National Institute of Biology, Ljubljana, Slovenia ABSTRACT: We have previously demonstrated that natural killer (NK) cells are the main immune effectors that can mediate selection and differentiation of different cancer stem cells and undifferentiated tumors via lysis and secreted or membrane-bound interferon-γ and tumor necrosis factor–α, respectively. This leads to growth inhibition and tumor metastasis curtailment. In this review, we present an overview of our findings on NK cell biology and its significance in selection and differentiation of stem-like tumors using in vitro and in vivo studies conducted in nonobese diabetic/severe combined immunodeficiency (scid)/interleukin-Rγ– –, humanized–bone-marrow/liver/thymus (hu-BLT) mice, and those of human cancer patients. Moreover, we present recent advances in NK cell expansion and therapeutic delivery and discuss the superiority of allogeneic supercharged NK cells over their autologous counterparts for cancer treatment. We review potential loss of NK cell numbers and function at neoplastic and preneoplastic stages of tumorigenesis as a potential mechanism for pancreatic cancer induction and progression. We believe that NK cells should be placed highly in the armamentarium of tumor immunotherapy due to their indispensable role in targeting cancer stem-like/poorly differentiated tumors and a variety of other key NK cell functions that are discussed in this report, including their role in CD8+ T-cell expansion and targeting gene knockout or dedifferentiated tumors. The combination of allogeneic supercharged NK cells and other immunotherapeutic strategies such as oncolytic viruses, antibody-dependent cellular cytotoxicity–inducing antibodies, checkpoint inhibitors, chimeric antigen receptor (CAR)-T cells and CAR-NK cells, chemotherapeutics, and radiotherapeutic strategies can be used for optimal eradication of tumors. To Read the Entire Publication Please Visit - http://www.dl.begellhouse.com/journals/2ff21abf44b19838,62b8a7004695c197,3d9b031b6a8cfac3.html
Can targeting NK cells, the key cytotoxic effectors, by Novel Coronavirus SARS-CoV-2 be the underlying reason for COVID-19 disease progression? Anahid Jewett, PhD, MPH Division of Oral Biology and Medicine, The Jane and Jerry Weintraub Center for Reconstructive Biotechnology, UCLA, Los Angeles, CA, USA, The Jonsson Comprehensive Cancer Center, UCLA School of Dentistry and Medicine, Los Angeles, CA, USA. Absract Coronavirus disease 2019 (COVID-19) poses a great public health challenge worldwide. While studies on SARS-CoV-2 effects on immune cell function continue to progress, we know very little about the significance of depletion of key immune effectors by the virus in the mortality and morbidity of the disease. This commentary reviews what is known thus far about the effect of virus on NK cells, the major cell type that is important in killing and removal of virally infected cells. It also provides a perspective on the necessity of comprehensive studies of NK cells in COVID-19 patients and animal models to better understand the role and significance of reported NK depletion and functional inactivation in disease morbidity and mortality, in hope to design effective therapeutic interventions for the disease. Coronavirus disease 2019 (COVID-19) poses a great public health threat, and presents a complex challenge for epidemiologists and public health officers around the planet, as the disease has shifted from a regional epidemic to a worldwide pandemic in a short period of time. The toll that the disease has had on the global level continues to skyrocket as the virus reaches all continents, except Antarctica, afflicting more than 180 countries. Initial reports of COVID-19 came from Wuhan, China in late December 2019, as patients began complaining about unexplained respiratory infections, which later was coined as “pneumonia of unknown etiology” (Cascella, Rajnik et al. 2020). Shortly after surfacing of the virus several independent laboratories identified the causative agent of COVID-19, ultimately naming it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (He, Deng et al. 2020, Lu, Zhao et al. 2020). While the search is continuing to uncover the infectious path of COVID-19, several key findings led the infectious disease experts to partly uncover the mechanisms of the original spread to humans. By phylogenetically comparing SARS-CoV-2 to other coronaviruses, it was noted that the new virus was highly identical to other coronaviruses that had originated from bats (Lu, Zhao et al. 2020, Yi, Lagniton et al. 2020). However, to date the complete transmission route remains elusive as an intermediate host of the COVID-19 virus remains to be identified. Despite the novelty of this particular strain of coronavirus, the COVID-19 virus is not without precedent. Outbreaks in the past decades, such as severe acute respiratory syndrome (SARS) and Middle East respiratory syndrome (MERS), identified viruses that fall into the same category of coronaviruses, which are single-stranded RNA viruses (+ssRNA) that morphologically have been determined to express crown-like spikes on their surfaces (1). However, the difference seen between prior species of coronaviruses and SARS-CoV-2 primarily lies in their respective symptom presentations in patients. Compared to SARS and MERS, the symptoms of COVID-19 are not presented earlier in the infectious cycle, which may be a reason for the greater ability of viral transmission in patients (Yi, Lagniton et al. 2020). The incubation period of the COVID-19 virus is relatively longer than that of SARS and MERs (7-14 days vs. 5.0-6.9 and 4.4-6.9, respectively) (Yi, Lagniton et al. 2020). Based on this observation it was recommended that patients and exposed individuals to undergo a 14-day medical observation period or quarantine. In addition to its longer incubation period, the mean reproductive number (R0) of SARS-CoV-2 has also been estimated to range from 2.20 to 3.58, indicating that each infected patient can on average transmit the disease to two to three other individuals (Zhao, Lin et al. 2020, Zhuang, Zhao et al. 2020). According to the available COVID-19 clinical data, most patients fall into the range of 30 to 79 years of age, although several cases have been identified in younger individuals and in children recently (Wu and McGoogan 2020). For infected patients, severity of symptoms has been classified as mild, severe, and critical. This spectrum of disease widely varies, as clinical presentation in infected individuals have ranged from asymptomatic infection to severe respiratory failure (He, Deng et al. 2020). Asymptomatic transmission of COVID-19 poses a great public health challenge in containment efforts, as previous reports have noted as much as 12.6% of case reports to be pre-symptomatic transmission (Du, Xu et al. 2020). However, the main characteristic symptoms of SARS-CoV-2 have included fevers, fatigue, dry cough and respiratory distress. Over two million cases have been identified thus far with SARS-CoV-2 worldwide, which has caused significant morbidity and mortality in the infected populations. This number will certainly continue to increase as more cases are seen in the hospitals in the months to come, even under strict adherence to public health policies and guidelines. Therefore, the world is continuing to embrace for the onslaught of more infected cases as the number of cases increases leading to both physical and economic hardship for populations worldwide. The disease will most likely continue to deplete the precious medical resources and threaten the safety of medical personnel and first responders if individuals continue to not take this disease seriously by loosely adhering to public health practices which call for isolation and social distancing and hand washing. One of the most troubling factors about this disease is the lack of adequate understanding of the virus and the mechanisms by which it mediates the underlying pathology in humans. The problem has been compounded by the limited ability of the research laboratories to conduct studies due to the implementation of social distancing since many academic university laboratories are either shut down or have been operating at a minimum capacity. Although the existing limited novel therapeutic strategies and research on potential vaccine are important directions, they will not be sufficient to provide adequate progress to fully understand the potential of the virus to infect patients and the underlying mechanisms by which the virus causes pathology. Containment efforts, through quarantines and social distancing, hand washing and wearing a mask are important directions to mitigate the spread of COVID-19. However, at the moment, we do not have the capability of large scale testing which would be necessary for the identification and isolation of asymptomatic and symptomatic patients to halt the chain of viral transmission. Therefore, until the existing public health measures are able to curtail the transmission and bring the disease somewhat under control, the research laboratories will not be able to fully engage in the studies of COVID-19 worldwide, thereby delaying the discoveries of more effective treatments and vaccines. Progression models of COVID-19 paint a dismal forecast for the duration of the outbreak, and therefore, warrant the discovery of novel treatments to alleviate disease symptoms that will supplement containment efforts. Researchers continue to scramble for viable treatments to alleviate symptoms of the disease and to eradicate the spread of the disease. The search for comprehensive treatment for COVID-19 has featured studies advocating for the potential use of the anti-malarial drugs, hydroxychloroquine, while others have gone down the immunologic path in support of monoclonal antibody therapy (Gautret, Lagier et al. 2020, Shanmugaraj, Siriwattananon et al. 2020). The development of a SARS-CoV-2 vaccine would utilize the adaptive immune system to combat symptoms in COVID-19 patients, along with providing a preventative measure for healthy individuals. However, current timelines estimate that vaccine development could take up to anywhere from 12 to 18 months. While studies on SARS-CoV-2’s effects on immune functions continue to progress, published studies concerning other coronaviruses may shed some light on how the immune system may be employed to mitigate COVID-19 symptoms. Based on experiences with coronaviruses in SARS and MERS, it has been suggested that the SARS-CoV-2 infection may also trigger major immunological changes, such as delayed or suppressed Type 1 IFN response and the influx of activated neutrophils and inflammatory monocytes/macrophages (Prompetchara, Ketloy et al. 2020). In addition, the effect of virus on host following infection has demonstrated severe changes in the proportion of different immune effectors (Wang, Nie et al. 2020). In particular, in the peripheral blood of patients that were infected with SARS, it was noted that there were significantly lower numbers of natural killer (NK) cells compared to healthy subjects (2004). Such a profile has also been extended to the immune responses of COVID-19 patients. A study of 452 COVID-19 patients demonstrated that the numbers of NK, B and T cells were significantly decreased, with more severe cases being associated with greater decreases in the numbers (Qin, Zhou et al. 2020), Please see the references (Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020) for in depth reviews on the biology and function of NK cells. Upon admission, the neutrophil counts were remarkably higher in patients with severe COVID-19 disease than in the mild cases, whereas the total lymphocyte counts were significantly lower in severe cases when compared to the mild cases (Qin, Zhou et al. 2020). In addition to NK cells, the numbers of T cells and CD8+ T cell were also decreased significantly in the mild and severe patients when compared to those of healthy controls. The numbers of NK cells as well as T cells and CD8+ T cells were significantly lower in patients exhibiting severe symptoms when compared to those with the mild symptoms and healthy controls (Zheng, Gao et al. 2020). Thus, a direct correlation could be seen with severe decrease in NK cell numbers and the extent of severity of the disease. Furthermore, the function of NK and CD8+ T cells was found to be suppressed along with the increased expression of NKG2A in COVID-19 patients (Zheng, Gao et al. 2020). More importantly, in patients convalescing after therapy, the numbers of NK and CD8+ T cells were restored with reduced expression of NKG2A. In addition, these results suggested that the functional exhaustion of cytotoxic lymphocytes was directly associated with severity of SRAS-CoV-2 infection. Hence, SARS-CoV-2 infection is likely to paralyze the antiviral immunity at an early stage and contribute to progression and severity of the disease (Zheng, Gao et al. 2020). In patients infected with SARS-CoV-2, NKG2A expression was increased significantly on NK and CD8+ T cells compared with those in healthy controls (Zheng, Gao et al. 2020). Lower percentages of CD107a+ NK, IFN-γ+ NK, IL-2+ NK, and TNF-α+ NK cells and decreased mean fluorescence intensities (MFI) of granzyme B+ NK cells were also reported in COVID-19 patients when compared to healthy controls (Zheng, Gao et al. 2020) . Taken together, these results clearly suggested the functional exhaustion of cytotoxic lymphocytes in COVID-19 patients (Zheng, Gao et al. 2020). Neutrophils are the most abundant white blood cells in the lung, and they are critical effectors against infections, in particular against bacterial infections, however they are also capable of inducing life-threatening morbidities. Moreover, Natural Killer cells are the most abundant lymphocytes in the lung, and therefore, play an important role not only in curtailment of infection but also in exertion of significant regulatory effect (Secklehner 2020). However, little is known regarding the specific mechanisms by which NK cells maintain local homeostasis. By using lung-intravital microscopy to directly visualize and quantify neutrophil and natural killer cell interaction within the lung of live mice, the authors reported in a preliminary study that NK cells were greatly responsible for the slower pace of scanning of endothelium by neutrophils over a large area, and they were able to reduce the number of neutrophils that accumulated in an LPS-triggered inflammatory challenge (Secklehner 2020). Indeed, depletion of NK cells in mice exhibited severe respiratory distress associated with protein-rich, high-permeability alveolar edema accompanied by neutrophil infiltration in myocardial infarction model (Yan, Hegab et al. 2014). Thus, NK cells are important effectors in not only combating the infection directly but also indirectly by activating the local inflammatory processes to curtail infection. In addition, they are also able to limit local immune activation in the lung to a manageable level without causing or allowing significant pathologies to be induced by other immune effectors. Thus NK cells are important in keeping the balance of immune activation in such a way that sufficient levels of activation will ensue to remove the infection in the presence of finely tuned inflammatory processes to avoid local tissue damage. As mentioned above the infectious agent of COVID-19 depletes NK cells in the peripheral blood and in lung tissues of patients, thereby, disabling and depleting the core immune effectors necessary to remove the virus and regulate uncontrolled immune activation. Indeed, NK cells are the army generals of the immune effectors which bring order and discipline to the infected tissue microenvironment. Without the NK cells it is likely that immune anarchy may ensue and result in the uncontrolled expansion and activation of other immune effectors (Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020) . We have previously shown that NK cells also curtail the numbers of CD4+ T cells and expand CD8+ T cells (Kaur, Topchyan et al. 2018, Kaur, Kozlowska et al. 2019) and (manuscript submitted). Therefore, lack of NK cells may also result in the decrease expansion of CD8+ T cells as seen in COVID-19 patients (Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020). Thus it is no surprise that COVID-19 patients have greater CD4/CD8 ratios as reported previously. The COVID-19 patients suffer from increased viral replication as well as uncontrolled inflammation resulting in cytokine storm and widespread tissue and organ damage (Bonow, Fonarow et al. 2020, McGonagle, Sharif et al. 2020). Natural killer (NK) cells are known to mediate cytotoxicity, and regulate both the innate and adaptive immune functions through the release of many pro- and anti-inflammatory growth factors, cytokines and chemokines (Fang, Xiao et al. 2017, Freud, Mundy-Bosse et al. 2017, Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020). They constitute 5-15% of the peripheral blood mononuclear cells (PBMCs), and are cytotoxic effectors in the blood of healthy individuals with the ability to recognize and lyse virally infected cells, including SARS-CoV-2 infected cells and a number of different cancer stem cells (CSCs) and undifferentiated or poorly differentiated tumors which constitute the most aggressive subpopulations of the tumors. Morphologically, NK cells are large granular lymphocytes that develop in the bone marrow. After development, the majority of NK cells are found in peripheral blood as the third largest lymphocyte population, next to B and T cells (Cooper, Fehniger et al. 2001). Moreover, NK cells are also found in the tissues such as in healthy skin, gut, lung, liver, lymphoid organs and uterus during pregnancy (Carrega and Ferlazzo 2012). NK cells have two different effector functions: cytotoxicity and cytokine release. In contrast to CD8+ cytotoxic T lymphocytes, NK cells do not need priming with antigen in order to kill their target cells. Their function is regulated by the sum of interactions between activating and inhibitory receptors on their surface and the ligands on the target cells (Pegram, Andrews et al. 2011). Ligands for NK activating receptors are expressed on fast proliferating cells that are virally infected or malignantly transformed. Cytotoxic activity of NK cells is executed by two distinct mechanisms. One is regulated by the cytotoxic granules containing perforin and granzymes. After the formation of the immune synapse between NK and target cells, cytotoxic granules are released. Perforin alters the permeability of the target cell membrane, allowing the entry of granzymes. The second pathway is interaction of ligands on NK cells with their respective cell death receptors on target cells. Target cell death can also be induced through antibody dependent cellular cytotoxicity (ADCC) (Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020). Indeed, NK cell mediated ADCC is likely one of the key mechanisms by which antibodies induced by the virus in recovered patients known as convalescent plasma or serum are able to alleviate the symptoms and improve the disease outcomes in infected and recovering patients (Shen, Wang et al. 2020) The second key effector function of NK cells is the release of cytokines and chemokines. Two major cytokines released by NK cells are IFN-γ and TNF-α (Abel, Yang et al. 2018, Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020). Released cytokines not only affect the function of innate and adaptive immune cells, but it can also impact the differentiation of both healthy and cancer cells. Similar to SRAS-CoV-2 infection in patients, decreased NK cell function in the tumor microenvironment, and peripheral blood of cancer patients as well as down-modulation of CD16 receptors on the surface of NK cells have been reported previously (Lai, Rabinowich et al. 1996, Kuss, Saito et al. 1999, Imai, Matsuyama et al. 2000, Bucklein, Adunka et al. 2016, Kaur, Cook et al. 2017, Kaur, Chang et al. 2018, Kaur, Topchyan et al. 2018). Decreased function of NK cells is associated with increased viral infection and cancer risk, whereas higher function was correlated with prevention of establishment and progression of infection and cancer (Jewett 2018, Jewett, Kos et al. 2018, Kaur, Nanut et al. 2018, Jewett, Kos et al. 2020). Indeed, older patients and those with immunosuppression are more susceptible to severe form of SRAS-CoV-2 infection, and are likely to die from it. Thus, it is no surprise that the same subsets of population of individuals are found to have lower expansion and functions of NK cells as reported previously (Hazeldine and Lord 2013, Gounder, Abdullah et al. 2018). Decreased NK and T cell numbers and function can be due to the activation induced cell death and/or direct infection of the immune cells by the virus. Indeed, recent studies indicated that similar to MERS-CoV infection, SRAS-CoV-2 also infects T cells through receptor-dependent, S-protein mediated membrane fusion and that the infection can be inhibited by EK1 peptide (Wang, Xu et al. 2020). Furthermore, the infection is abortive since SRAS-CoV-2 does not have the capability to replicate in the T cells (Wang, Xu et al. 2020). With promising studies demonstrating significant decreases and functional deficiencies in immune cell populations in particular the NK cells in COVID-19 patients, immunotherapy-based treatments using NK cells and CD8+ T cells and/or enhancement of the proliferation and function of NK cells in patients may present a significant and viable avenue towards mitigating disease establishment and progression. References: (2004). "The involvement of natural killer cells in the pathogenesis of severe acute respiratory syndrome." Am J Clin Pathol 121(4): 507-511. Abel, A. M., C. Yang, M. S. Thakar and S. Malarkannan (2018). "Natural Killer Cells: Development, Maturation, and Clinical Utilization." Front Immunol 9: 1869. Bonow, R. O., G. C. Fonarow, P. T. O'Gara and C. W. Yancy (2020). "Association of Coronavirus Disease 2019 (COVID-19) With Myocardial Injury and Mortality." JAMA Cardiol. Bucklein, V., T. Adunka, A. N. Mendler, R. Issels, M. Subklewe, J. C. Schmollinger and E. Noessner (2016). "Progressive natural killer cell dysfunction associated with alterations in subset proportions and receptor expression in soft-tissue sarcoma patients." Oncoimmunology 5(7): e1178421. Carrega, P. and G. Ferlazzo (2012). "Natural killer cell distribution and trafficking in human tissues." Front Immunol 3: 347. Cascella, M., M. Rajnik, A. Cuomo, S. C. Dulebohn and R. Di Napoli (2020). Features, Evaluation and Treatment Coronavirus (COVID-19). StatPearls. Treasure Island (FL). Cooper, M. A., T. A. Fehniger and M. A. Caligiuri (2001). "The biology of human natural killer-cell subsets." Trends Immunol 22(11): 633-640. Du, Z., X. Xu, Y. Wu, L. Wang, B. J. Cowling and L. A. Meyers (2020). "Serial Interval of COVID-19 among Publicly Reported Confirmed Cases." Emerg Infect Dis 26(6). Fang, F., W. Xiao and Z. Tian (2017). "NK cell-based immunotherapy for cancer." Semin Immunol 31: 37-54. Freud, A. G., B. L. Mundy-Bosse, J. Yu and M. A. Caligiuri (2017). "The Broad Spectrum of Human Natural Killer Cell Diversity." Immunity 47(5): 820-833. Gautret, P., J. C. Lagier, P. Parola, V. T. Hoang, L. Meddeb, M. Mailhe, B. Doudier, J. Courjon, V. Giordanengo, V. E. Vieira, H. T. Dupont, S. Honore, P. Colson, E. Chabriere, B. La Scola, J. M. Rolain, P. Brouqui and D. Raoult (2020). "Hydroxychloroquine and azithromycin as a treatment of COVID-19: results of an open-label non-randomized clinical trial." Int J Antimicrob Agents: 105949. Gounder, S. S., B. J. J. Abdullah, N. Radzuanb, F. Zain, N. B. M. Sait, C. Chua and B. Subramani (2018). "Effect of Aging on NK Cell Population and Their Proliferation at Ex Vivo Culture Condition." Anal Cell Pathol (Amst) 2018: 7871814. Hazeldine, J. and J. M. Lord (2013). "The impact of ageing on natural killer cell function and potential consequences for health in older adults." Ageing Res Rev 12(4): 1069-1078. He, F., Y. Deng and W. Li (2020). "Coronavirus disease 2019: What we know?" J Med Virol. Imai, K., S. Matsuyama, S. Miyake, K. Suga and K. Nakachi (2000). "Natural cytotoxic activity of peripheral-blood lymphocytes and cancer incidence: an 11-year follow-up study of a general population." Lancet 356(9244): 1795-1799. Jewett, A. (2018). "Editorial overview: Tumour immunology: Are we on the path to win the battle against cancer through immunotherapy?" Curr Opin Immunol 51: vii-ix. Jewett, A., J. Kos, Y. Fong, M. W. Ko, T. Safaei, M. Perisic Nanut and K. Kaur (2018). "NK cells shape pancreatic and oral tumor microenvironments; role in inhibition of tumor growth and metastasis." Semin Cancer Biol 53: 178-188. Jewett, A., J. Kos, K. Kaur, T. Safaei, C. Sutanto, W. Chen, P. Wong, A. K. Namagerdi, C. Fang, Y. Fong and M. W. Ko (2020). "Natural Killer Cells: Diverse Functions in Tumor Immunity and Defects in Pre-neoplastic and Neoplastic Stages of Tumorigenesis." Mol Ther Oncolytics 16: 41-52. Kaur, K., H. H. Chang, P. Topchyan, J. M. Cook, A. Barkhordarian, G. Eibl and A. Jewett (2018). "Deficiencies in Natural Killer Cell Numbers, Expansion, and Function at the Pre-Neoplastic Stage of Pancreatic Cancer by KRAS Mutation in the Pancreas of Obese Mice." Front Immunol 9: 1229. Kaur, K., J. Cook, S. H. Park, P. Topchyan, A. Kozlowska, N. Ohanian, C. Fang, I. Nishimura and A. Jewett (2017). "Novel Strategy to Expand Super-Charged NK Cells with Significant Potential to Lyse and Differentiate Cancer Stem Cells: Differences in NK Expansion and Function between Healthy and Cancer Patients." Front Immunol 8: 297. Kaur, K., A. K. Kozlowska, P. Topchyan, M. W. Ko, N. Ohanian, J. Chiang, J. Cook, P. O. Maung, S. H. Park, N. Cacalano, C. Fang and A. Jewett (2019). "Probiotic-Treated Super-Charged NK Cells Efficiently Clear Poorly Differentiated Pancreatic Tumors in Hu-BLT Mice." Cancers (Basel) 12(1). Kaur, K., M. P. Nanut, M. W. Ko, T. Safaie, J. Kos and A. Jewett (2018). "Natural killer cells target and differentiate cancer stem-like cells/undifferentiated tumors: strategies to optimize their growth and expansion for effective cancer immunotherapy." Curr Opin Immunol 51: 170-180. Kaur, K., P. Topchyan, A. K. Kozlowska, N. Ohanian, J. Chiang, P. O. Maung, S. H. Park, M. W. Ko, C. Fang, I. Nishimura and A. Jewett (2018). "Super-charged NK cells inhibit growth and progression of stem-like/poorly differentiated oral tumors in vivo in humanized BLT mice; effect on tumor differentiation and response to chemotherapeutic drugs." Oncoimmunology 7(5): e1426518. Kuss, I., T. Saito, J. T. Johnson and T. L. Whiteside (1999). "Clinical significance of decreased zeta chain expression in peripheral blood lymphocytes of patients with head and neck cancer." Clin Cancer Res 5(2): 329-334. Lai, P., H. Rabinowich, P. A. Crowley-Nowick, M. C. Bell, G. Mantovani and T. L. Whiteside (1996). "Alterations in expression and function of signal-transducing proteins in tumor-associated T and natural killer cells in patients with ovarian carcinoma." Clin Cancer Res 2(1): 161-173. Lu, R., X. Zhao, J. Li, P. Niu, B. Yang, H. Wu, W. Wang, H. Song, B. Huang, N. Zhu, Y. Bi, X. Ma, F. Zhan, L. Wang, T. Hu, H. Zhou, Z. Hu, W. Zhou, L. Zhao, J. Chen, Y. Meng, J. Wang, Y. Lin, J. Yuan, Z. Xie, J. Ma, W. J. Liu, D. Wang, W. Xu, E. C. Holmes, G. F. Gao, G. Wu, W. Chen, W. Shi and W. Tan (2020). "Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding." Lancet 395(10224): 565-574. McGonagle, D., K. Sharif, A. O'Regan and C. Bridgewood (2020). "The Role of Cytokines including Interleukin-6 in COVID-19 induced Pneumonia and Macrophage Activation Syndrome-Like Disease." Autoimmun Rev: 102537. Pegram, H. J., D. M. Andrews, M. J. Smyth, P. K. Darcy and M. H. Kershaw (2011). "Activating and inhibitory receptors of natural killer cells." Immunol Cell Biol 89(2): 216-224. Prompetchara, E., C. Ketloy and T. Palaga (2020). "Immune responses in COVID-19 and potential vaccines: Lessons learned from SARS and MERS epidemic." Asian Pac J Allergy Immunol 38(1): 1-9. Qin, C., L. Zhou, Z. Hu, S. Zhang, S. Yang, Y. Tao, C. Xie, K. Ma, K. Shang, W. Wang and D. S. Tian (2020). "Dysregulation of immune response in patients with COVID-19 in Wuhan, China." Clin Infect Dis. Secklehner, J. (2020). "Pulmonary natural killer cells control neutrophil intravascular motility and response to acute inflammation." Biorexiv. Shanmugaraj, B., K. Siriwattananon, K. Wangkanont and W. Phoolcharoen (2020). "Perspectives on monoclonal antibody therapy as potential therapeutic intervention for Coronavirus disease-19 (COVID-19)." Asian Pac J Allergy Immunol 38(1): 10-18. Shen, C., Z. Wang, F. Zhao, Y. Yang, J. Li, J. Yuan, F. Wang, D. Li, M. Yang, L. Xing, J. Wei, H. Xiao, Y. Yang, J. Qu, L. Qing, L. Chen, Z. Xu, L. Peng, Y. Li, H. Zheng, F. Chen, K. Huang, Y. Jiang, D. Liu, Z. Zhang, Y. Liu and L. Liu (2020). "Treatment of 5 Critically Ill Patients With COVID-19 With Convalescent Plasma." JAMA. Wang, F., J. Nie, H. Wang, Q. Zhao, Y. Xiong, L. Deng, S. Song, Z. Ma, P. Mo and Y. Zhang (2020). "Characteristics of peripheral lymphocyte subset alteration in COVID-19 pneumonia." J Infect Dis. Wang, X., W. Xu, G. Hu, S. Xia, Z. Sun, Z. Liu, Y. Xie, R. Zhang, S. Jiang and L. Lu (2020). "SARS-CoV-2 infects T lymphocytes through its spike protein-mediated membrane fusion." Cell Mol Immunol. Wu, Z. and J. M. McGoogan (2020). "Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72314 Cases From the Chinese Center for Disease Control and Prevention." JAMA. Yan, X., A. E. Hegab, J. Endo, A. Anzai, T. Matsuhashi, Y. Katsumata, K. Ito, T. Yamamoto, T. Betsuyaku, K. Shinmura, W. Shen, E. Vivier, K. Fukuda and M. Sano (2014). "Lung natural killer cells play a major counter-regulatory role in pulmonary vascular hyperpermeability after myocardial infarction." Circ Res 114(4): 637-649. Yi, Y., P. N. P. Lagniton, S. Ye, E. Li and R. H. Xu (2020). "COVID-19: what has been learned and to be learned about the novel coronavirus disease." Int J Biol Sci 16(10): 1753-1766. Zhao, S., Q. Lin, J. Ran, S. S. Musa, G. Yang, W. Wang, Y. Lou, D. Gao, L. Yang, D. He and M. H. Wang (2020). "Preliminary estimation of the basic reproduction number of novel coronavirus (2019-nCoV) in China, from 2019 to 2020: A data-driven analysis in the early phase of the outbreak." Int J Infect Dis 92: 214-217. Zheng, M., Y. Gao, G. Wang, G. Song, S. Liu, D. Sun, Y. Xu and Z. Tian (2020). "Functional exhaustion of antiviral lymphocytes in COVID-19 patients." Cell Mol Immunol. Zhuang, Z., S. Zhao, Q. Lin, P. Cao, Y. Lou, L. Yang and D. He (2020). "Preliminary estimation of the novel coronavirus disease (COVID-19) cases in Iran: A modelling analysis based on overseas cases and air travel data." Int J Infect Dis.